09 Jan ITHS Profile: Centering Mental Health in Rural Idaho Garners NIH Award
The ITHS profile series is meant to shine a deserving spotlight on individuals or programs within ITHS doing critical work across the vast spectrum of translational science. For this installment, we connected with Dr. Kelly McGrath, MD, MS, to discuss the $200,000 award from the National Institutes of Health (NIH) and National Heart, Lung, and Blood Institute (NHLBI) through the highly competitive NIH Build UP Trust Challenge. Dr. McGrath serves as Chief Medical Officer at two Idaho Critical Access Hospitals: Clearwater Valley Health and St. Mary’s Health; and is the co-director of the ITHS Rural Health Initiative.
In this interview, Dr. McGrath discusses breaking down barriers to healthcare access and how meeting people where they were was key to this project’s success.
What kind of work do you do?
McGrath: Fundamentally, we work to meet the healthcare needs of the rural and frontier populations of North Central Idaho. We are a system of two rural critical access hospitals and 8 clinics that serve a population of approximately 28,000 people dispersed over a large area. This population tends to be older, sicker and economically not as well off as the rest of the country. We strive to be a leader in rural healthcare and believe that there are new ways that we can best meet the needs of this population. Our hope also is that these methods can be generalized to other communities that face similar challenges.
Working in a resource-contained environment, such as we have in rural healthcare, it is hard to innovate. Much of our effort is focused on just keeping our doors open and the fundamental actions necessary to deliver healthcare. This is why our partnership with the ITHS has been so important. That relationship has served as a catalyst for needed innovation to improve patient outcomes.
How did you first get connected with ITHS?
McGrath: About eleven years ago we started working with the ITHS on an opioid safety project. This project resonated with us because, like most of the country, we were challenged around chronic opioid prescribing. That project was pivotal in changing to our local practice regarding chronic opioid use. Subsequently, we have been involved in about ten projects which have helped us evolve into a small, rural Learning Health System. Our core project has been working with the ITHS and our communities in the Rural Health Initiative. This project creates synergy between academic medicine, community and our local healthcare system.
ITHS has been the engine to drive innovation in our organization and develop new pathways to improve health outcomes in rural Idaho.
What motivated you to address mental health care access and barriers in rural Idaho?
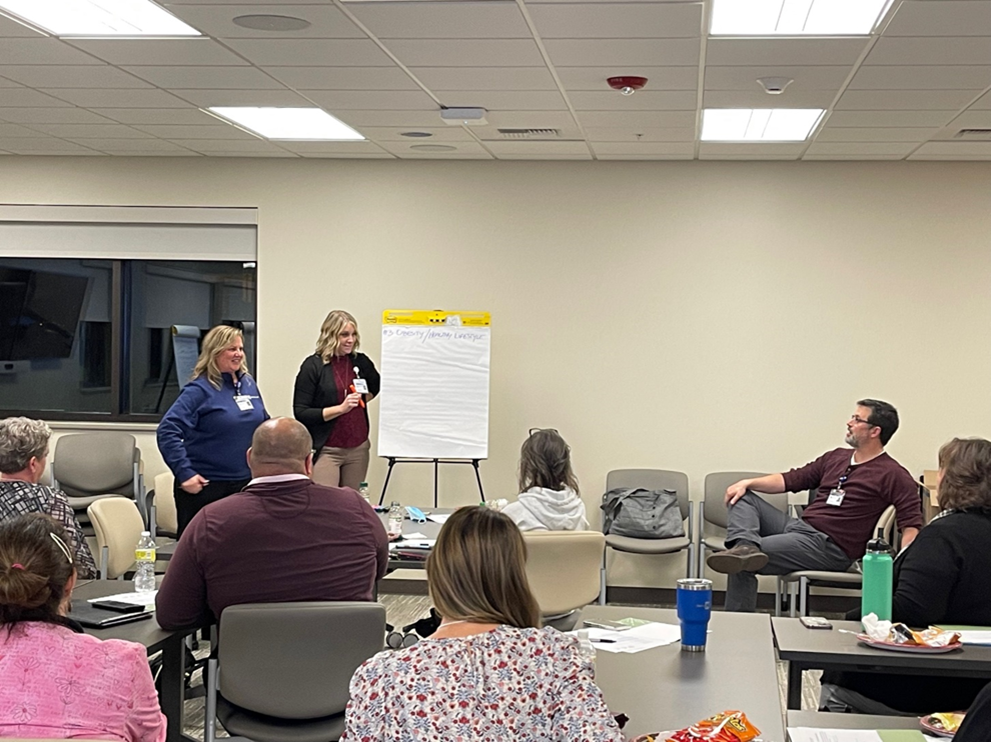
McGrath: Our partnership with the community brought the focus on this work. Through the Rural Health Initiative, we met with community stakeholders to identify healthcare priorities. After reviewing data compiled by ITHS, stakeholder discussion, and conducting a community survey of priorities, it was clear that this was the top issue. To me, the most compelling moment was
during the stakeholder community meeting. After defining deaths of despair, I asked those in the room if they personally were connected to someone who had died from these causes. Sadly, nearly all the hands in the room went up.
Access to mental health services in Idaho is amongst the worst in the nation, and we have a large percentage of rural and frontier populations in our state. This makes it difficult to provide care due to geography and the dispersed population. Also, the Intermountain West also has some of the highest suicide rates. We felt that there was an opportunity to deliver care that better met the needs of our population. This led us to the work that we have been recognized for with the Build Up Trust award.
Can you tell us more about the project that won the NIH Build UP Trust Challenge?
McGrath: Yes, we started by recognizing a big piece of the problem, which is that we have a dispersed and isolated population that does not necessarily have access to traditional healthcare, particularly mental health care. We had previously demonstrated improved outcomes in diabetes care through the work of our community health workers and population health teams. We speculated that the same model of care could be used to address gaps in mental health within our community.
Our previous experience revealed that community members generally had a trusting relationship with our community health workers. We felt that this was just the right platform to help people who were not being reached by our traditional healthcare system. We met people where they were, whether at food distribution sites, health promotional events or county fairs to screen for mental health issues. Those who screened positive were offered additional care and given tools to support their psychological health.
The Build Up Trust Challenge incorporates two phases: the first phase with an award of approximately $40,000 to implement the program; the second phase is the primary award of $200,000 to help sustain the work. During the first phase, in response to the community input, we designed and implemented the screening and intervention pathways. Since we were engaging a population who did not typically access traditional healthcare, trust was a foundational piece of this work. To assess this, community health workers surveyed community members’ trust in our local healthcare system. Just over 80% of people identified our system as one they trust. The results validated that, even outside of the standard healthcare environment, community health workers can be an effective means to establish trust. We learned that people are willing to engage in mental health screening and referrals when trust is established in this way.
Can you tell us any stories about the people you hope this reaches – and why you hope this helps them?
McGrath: The people that we hope to help are those who we are not reaching right now. It is devastating when you hear that someone in the community has taken their life, and particularly if they never accessed our healthcare system for help. My hope is that we will intervene earlier to support those who need it.
How will you be incorporating community concerns & priorities into your plan?
McGrath: As mentioned, it was through community partnerships that we identified these needs and priorities. We use the community partnership as our north star. We will continue to build and maintain community partnerships to inform our health care priorities.
We use the community partnership as our north star.
Why is the Build Up Trust program so important for projects like yours?
McGrath: Build Up Trust fosters innovative care models to address unmet healthcare needs. Without this support and the partnership with the ITHS, it is hard to find the optimal ways to care for our community. Programs like these make it possible to improve, even in resource-constrained environments.
What does success look like to you and what do you hope this project accomplishes?
McGrath: Economic hardships should not be a barrier to health care access. Hopefully, this approach allows us to more effectively help people in need and reduce barriers tied to culture and economic hardship. That would be a meaningful outcome.
Economic hardships should not be a barrier to health care access
Congratulations to the team and Dr. McGrath!