14 Apr Study Finds Public Support for Research on Medical Practices
New findings from the Institute of Translational Health Sciences study, “Attitudes About the Ethics of Research on Medical Practices (ROMP),” have added the voice of potential research participants to the ongoing debate about the informed consent process in studies where the lines between research and clinical practice are blurred.
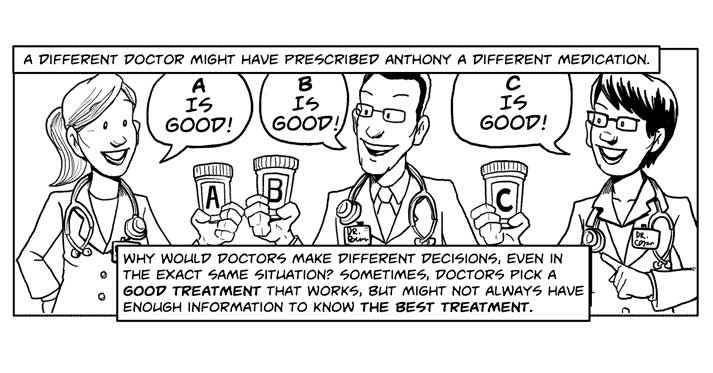
It is standard practice for researchers to disclose potential risks of research to patients prior to obtaining their consent to participate in a clinical trial for new drugs. However, what to say about risks for randomized trials that compare approved treatments to resolve uncertainty is more complicated because risks of usual treatments will be present even for those who are not participating in the research.
The ROMP Ethics study was launched to assess the attitudes of potential participants about risks, notification preferences, and consent in these types of studies. The study took place against the backdrop of new draft guidance from the U.S. Office for Human Research Protections (OHRP), which states that the risks of research and risks of treatment should now be viewed as one and the same.
The study findings, which were recently published in Annals of Internal Medicine, showed strong support among the public for research seeking to determine which approved treatments work better. The findings also provided additional clarity on potential participants’ preferences when it comes to securing consent to participate and the disclosure of risks associated with being in a these studies.
“Patients want to be told about this research, whether it involves reviewing their medical records or randomizing them to different treatments,” explained lead ITHS researcher Dr. Benjamin Wilfond, Director of the Treuman Katz Center for Pediatric Bioethics at Seattle Children’s Research Institute and Professor and Chief of the Division of Bioethics in the Department of Pediatrics at the University of Washington School of Medicine. “While they prefer written permission for all research, most patients are comfortable with just verbal permission or notification, with more willing to accept less elaborate approaches if doing so would allow research to go forward.”
The ROMP study, which is a collaborative effort between ITHS and Spectrum at Stanford University, reached its findings by surveying 1,095 adults located across the U.S. Survey respondents were each presented with key features of research on medical practices via three narrative videos. These three-minute videos explained in plain language the factors that influence variation in clinical practice, randomization and medical record review, and different approaches to notifying patients about research and obtaining consent to participate. Respondents were then asked about their trust in physicians and health systems, their understanding of research on medical practices, attitudes towards and risks and consent, and their willingness to participate in research on medical practices.
“The findings suggest that OHRP makes too much of distinction between medical record review and randomized trials,” shared lead Spectrum researcher Dr. David Magnus, Director of the Stanford Center for Biomedical Ethics and Thomas A. Raffin Professor of Medicine and Biomedical Ethics and Professor of Pediatrics at Stanford University. “The OHRP guidance will make it more difficult to conduct some of these studies, and it is clear this is not consistent with patient views.”
Please visit www.rompethics.org to learn more about the ROMP study or to see the three videos that were viewed by survey respondents.